Neuropathic pain has no immediate cause – research on a brain receptor may help stop this hard-to-treat condition
- Neuropathic pain, which affects 10% of the US population, has no clear cause and can be debilitating, leading to depression, anxiety, social isolation, and a deep sense of helplessness.
- Research on a brain receptor called GluD1 suggests that it plays a crucial role in shaping pain circuits and may offer a way to repair the pain processing network itself with fewer side effects and less risk of addiction than current treatments.
- GluD1 helps organize synapses, directing where connections form and how strong they become, and its activity is linked to persistent pain; restoring GluD1 activity can reduce pain.
- Disruptions to GluD1 activity lead to chaotic communication between brain cells, causing neurons to misfire and overreact, resulting in increased pain sensitivity both physically and emotionally.
- A study found that reactivating GluD1 activity with a protein called cerebellin-1 eased chronic pain in mice without producing side effects, suggesting a potential new approach for treating neuropathic pain.
Pain is easy to understand until it isn’t. A stubbed toe or sprained ankle hurts, but it makes sense because the cause is clear and the pain fades as you heal.
But what if the pain didn’t go away? What if even a breeze felt like fire, or your leg burned for no reason at all? When pain lingers without a clear cause, that’s neuropathic pain.
We are neuroscientists who study how pain circuits in the brain and spinal cord change over time. Our work focuses on the molecules that quietly reshape how pain is felt and remembered.
We didn’t fully grasp how different neuropathic pain was from injury-related pain until we began working in a lab studying it. Patients spoke of a phantom pain that haunted them daily – unseen, unexplained and life-altering.
These conversations shifted our focus from symptoms to mechanisms. What causes this ghost pain to persist, and how can we intervene at the molecular level to change it?
More than just physical pain
Neuropathic pain stems from damage to or dysfunction in the nervous system itself. The system that was meant to detect pain becomes the source of it, like a fire alarm going off without a fire. Even a soft touch or breeze can feel unbearable.
Neuropathic pain doesn’t just affect the body – it also alters the brain. Chronic pain of this nature often leads to depression, anxiety, social isolation and a deep sense of helplessness. It can make even the most routine tasks feel unbearable.
About 10% of the U.S. population – tens of millions of people – experience neuropathic pain, and cases are rising as the population ages. Complications from diabetes, cancer treatments or spinal cord injuries can lead to this condition. Despite its prevalence, doctors often overlook neuropathic pain because its underlying biology is poorly understood.

Kate Wieser/Moment via Getty Images
There’s also an economic cost to neuropathic pain. This condition contributes to billions of dollars in health care spending, missed workdays and lost productivity. In the search for relief, many turn to opioids, a path that, as seen from the opioid epidemic, can carry its own devastating consequences through addiction.
GluD1: A quiet but crucial player
Finding treatments for neuropathic pain requires answering several questions. Why does the nervous system misfire in this way? What exactly causes it to rewire in ways that increase pain sensitivity or create phantom sensations? And most urgently: Is there a way to reset the system?
This is where our lab’s work and the story of a receptor called GluD1 comes in. Short for glutamate delta-1 receptor, this protein doesn’t usually make headlines. Scientists have long considered GluD1 a biochemical curiosity, part of the glutamate receptor family, but not known to function like its relatives that typically transmit electrical signals in the brain.
Instead, GluD1 plays a different role. It helps organize synapses, the junctions where neurons connect. Think of it as a construction foreman: It doesn’t send messages itself, but directs where connections form and how strong they become.
This organizing role is critical in shaping the way neural circuits develop and adapt, especially in regions involved in pain and emotion. Our lab’s research suggests that GluD1 acts as a molecular architect of pain circuits, particularly in conditions like neuropathic pain where those circuits misfire or rewire abnormally. In parts of the nervous system crucial for pain processing like the spinal cord and amygdala, GluD1 may shape how people experience pain physically and emotionally.
Fixing the misfire
Across our work, we found that disruptions to GluD1 activity is linked to persistent pain. Restoring GluD1 activity can reduce pain. The question is, how exactly does GluD1 reshape the pain experience?
In our first study, we discovered that GluD1 doesn’t operate solo. It teams up with a protein called cerebellin-1 to form a structure that maintains constant communication between brain cells. This structure, called a trans-synaptic bridge, can be compared to a strong handshake between two neurons. It makes sure that pain signals are appropriately processed and filtered.
But in chronic pain, the bridge between these proteins becomes unstable and starts to fall apart. The result is chaotic. Like a group chat where everyone is talking at once and nobody can be heard clearly, neurons start to misfire and overreact. This synaptic noise turns up the brain’s pain sensitivity, both physically and emotionally. It suggests that GluD1 isn’t just managing pain signals, but also may be shaping how those signals feel.
What if we could restore that broken connection?
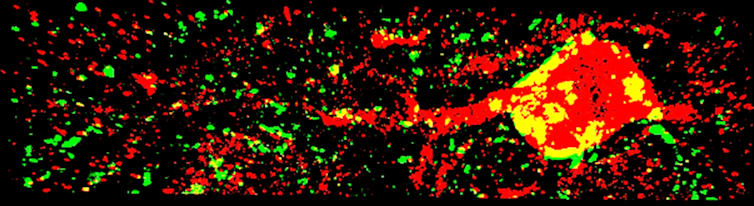
Pooja Shree Chettiar and Siddhesh Sabnis/Dravid Lab at Texas A&M University, CC BY-SA
In our second study, we injected mice with cerebellin-1 and saw that it reactivated GluD1 activity, easing their chronic pain without producing any side effects. It helped the pain processing system work again without the sedative effects or disruptions to other nerve signals that are common with opioids. Rather than just numbing the body, reactivating GluD1 activity recalibrated how the brain processes pain.
Of course, this research is still in the early stages, far from clinical trials. But the implications are exciting: GluD1 may offer a way to repair the pain processing network itself, with fewer side effects and less risk of addiction than current treatments.
For millions living with chronic pain, this small, peculiar receptor may open the door to a new kind of relief: one that heals the system, not just masks its symptoms.
![]()
The authors do not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
